Tiffany Lee, April 16, 2020
NU researchers develop strategy for ventilator sharing
One of the most highly publicized problems during the COVID-19 pandemic has been a potential shortage of ventilators, the lifesaving machines that help people breathe.
Current estimates suggest that roughly 5% of COVID-19 patients develop acute respiratory distress syndrome, or ARDS, a condition that mandates ventilator use. With about 173,000 ventilators available across the nation, and millions of Americans expected to contract the virus, scarcity of the machines is a viable reality.
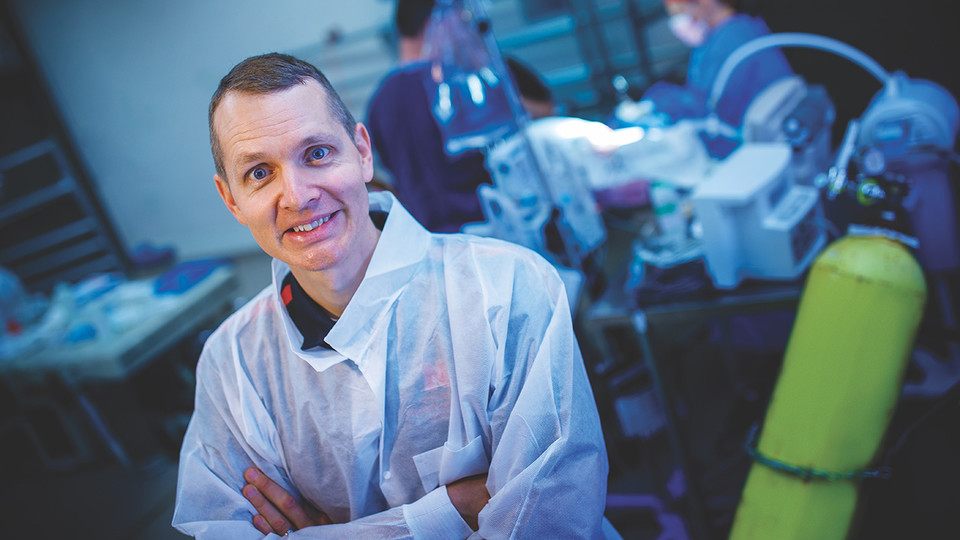
The problem captured the attention of Benjamin Terry, an engineer at the University of Nebraska–Lincoln, and Keely Buesing, a trauma critical care surgeon at the University of Nebraska Medical Center. Building on their combined expertise and ongoing research collaboration focused on developing therapies and devices to treat ARDS, the team has developed a strategy for stacking two patients on the same ventilator.
University of Nebraska–Lincoln graduate students Nathaniel Zollinger, Benjamin Wankum and Riley Reynolds, along with Husker alumna Andrea McCain, also made major contributions to the project.
Their approach isn’t mechanically fancy — it relies on standard tubing and widely available hardware store supplies — but it provides a viable option for clinicians during a crisis. Though Nebraska is not currently projected to a face a ventilator shortage, Buesing said it’s reassuring to have a potential solution in place and is something to offer other hard-hit communities.
“I’ve talked to my colleagues, and we agree that if we’re looking at two patients and their families, we don’t want to have to make a decision as to who gets the ventilator,” said Buesing, associate professor of surgery. “Now we have something possible so we won’t have to make those decisions.”
Terry and Buesing’s setup is innovative in that it tackles the core problem with split ventilation: patient mismatch, which is when patients of different sizes, diagnoses or states of disease progression are candidates for sharing the same ventilator. Of these factors, Buesing said the third — varying degrees of lung pathology — is the most challenging to frontline clinicians.
That’s because different levels of pathology lead to different degrees of lung compliance, which is a measure of the organs’ ability to stretch and expand. Sharing a ventilator between patients with different lung compliances presents serious challenges. The lungs of the sicker patient take in less oxygen because they are stiffer and harder to inflate, driving the healthier patient’s lungs to take in more than they need. Sustained hyperventilation is dangerous for the lungs, akin to weakening a balloon by overfilling it too many times.
This is why simply splitting a ventilator is feasible and safe only when two patients are a near-perfect match. During a crisis, finding these ideal pairings is unlikely.
“A lot of the literature shows that splitting a ventilator circuit without any augmentations can work if you have two people with perfectly matched disease needs,” Buesing said. “But that’s a perfect case scenario that is not likely to happen.”
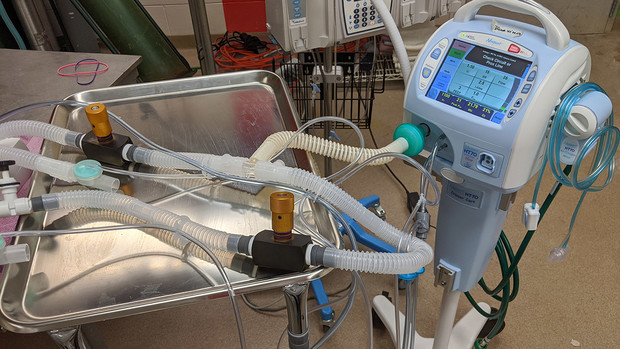
Terry and Buesing’s solution is the use of a simple, widely available tool: a variable flow restrictor. The device, basic enough that it’s stocked at big-box retailers, would allow health care practitioners to decrease the oxygen volume to the healthier patient, avoiding hyperinflation.
“We’re using the same tubing system you can buy off the shelf, and just modifying it a little bit,” said Terry, associate professor of mechanical and materials engineering. “You could essentially do this setup with stuff from Home Depot, though we’ve used higher-quality parts.”
Under their setup, the ventilator is initially split using standard tubing. The flow restrictors are then inserted in the appropriate places for both patients, and a three-way valve is attached to the ventilator’s pressure lines. This configuration enables the clinician to decrease the oxygen volume to the healthier person without undercutting the sicker person’s needs. And adding a flow restrictor to both patients’ equipment confers flexibility to adapt to a fluid situation.
“You never know what’s going to happen in a couple of hours,” Terry said. “One patient might improve and you would need to reverse your strategy.”
With funding from Nebraska’s College of Engineering and Office of Research and Economic Development, the team has run two successful trials using the setup and hopes to eventually publish results after further experiments.
Amid the current pandemic, safety concerns led professional medical organizations to release a consensus statement advising against ventilator sharing. Terry and Buesing agree that the practice is never ideal and that their setup has downsides, including an increased need for human labor to handle setup and monitoring, a potential strain on the ventilators’ mechanical capacity and the risk of cross contamination between patients, among others.
But in an urgent situation where other solutions are unavailable, Buesing said she’s optimistic the team’s approach could be successful in mitigating at least a portion of the mismatch problem. She and Terry hope their strategy can help the medical and research communities address a pressing problem and assure Nebraskans their needs can be met.
Buesing said contributing to the project is one way she is giving back to a state that’s been overwhelmingly supportive during the pandemic.
“The outpouring has been amazing,” she said. “People have been donating masks and gear and giving thanks to us on the front lines. It gets me a little bit emotional. It’s nice, heartwarming and lifts our spirits.”