Tiffany Lee, January 23, 2019 | View original publication
Nebraska researchers readying revolutionary stroke treatment
Researchers at the University of Nebraska-Lincoln are readying to bring a revolution to acute ischemic stroke care.
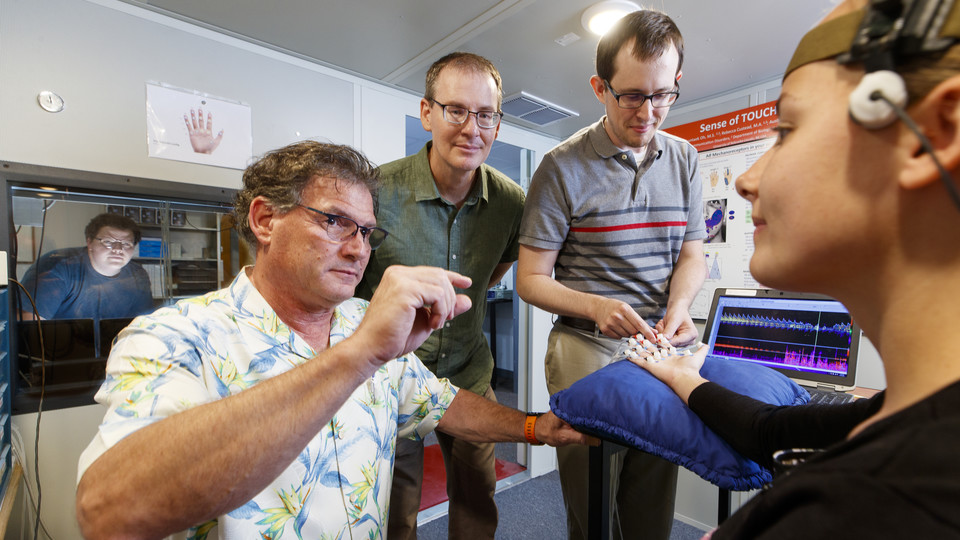
Steven Barlow and Greg Bashford, along with graduate students Ben Hage and Jake Greenwood, recently published findings in the Journal of Neuroimaging that demonstrated the technologies they have developed to evoke somatosensory stimulation significantly raised cerebral blood flow to areas typically affected by large vessel ischemic stroke.
These findings, along with previous research by Barlow’s and Bashford’s teams, has led to a partnership with CHI Immanuel Medical Center in Omaha to utilize the technology with patients affected by cerebrovascular stroke.
Barlow said he, Bashford and a team of graduate students will soon bring somatosensory stimulation and improved blood flow monitoring to stroke sufferers in clinical trials.
Ischemic stroke is caused by a clot or narrowing of the artery, which obstructs the blood pathways in the brain, depriving cells of the oxygen needed to stay alive. In the Neuroimaging study, the researchers produced precise stimulation to the brain of healthy adults using the Galileo TAC-Cell Array, and monitored cerebral blood flow in real time with functional transcranial Doppler ultrasound, or fTCD, which uses novel blood flow analysis algorithms developed at Nebraska.
The researchers noted increases in the velocity of brain blood flow of up to 20 percent, which is a massive change, Bashford said. Barlow said this change in blood flow has been shown in animal models to provide neuroprotection, by forcing the brain to reroute blood supply to an area affected by stroke.
“One of the goals of neurology when dealing with stroke patients is to figure out therapies that can promote collateral blood flow, in an effort to preserve brain function,” Barlow, Corwin Moore Professor of Special Education and Communication Disorders and associate director of the Center for Brain, Biology and Behavior, said. “They have this phrase in the stroke literature, ‘time is brain.’ Every minute, you lose approximately 2 million neurons and 14 billion synapses as the stroke evolves, so we’re really focused on neuroprotection in the acute phase with this approach.”
Barlow invented the Galileo as an investigative machine, but quickly saw its potential for controlled stimulation to offset brain injury. Galileo utilizes pressurized air as a non-invasive method of brain stimulation.
The Galileo had significant performance limitations in the challenging environment of acute stroke care, Barlow said. It has been redesigned by Barlow and graduate student Jake Greenwood as the pTACS somatosensory stimulator, and the team has applied for a patent through NUTech. The new machine is now much smaller, the size of a lunch box, is mobilized through battery power and is operationally silent. The new machine is accepted by stroke care specialists for use in emergency department and intensive care unit.
The stimulator produces air pulses at supersonic speeds that are sent through small plastic tubes into tiny capsules that are adhered to the hands or face to create a nerve response. The capsules are applied to the skin in specific patterns and speeds to activate the brain’s cerebral cortex and cerebellum and increase blood flow.
Bashford, Professor of Biological Systems Engineering and a faculty affiliate at CB3, invented a custom fixation device for fTCD, along with blood flow detection and analysis routines from data acquired that complements the somatosensory stimulation, allowing researchers and doctors to monitor blood flow in real-time from particular areas of the brain. The two researchers put together an interdisciplinary team of scholars to combine the two technologies.
Previously, doctors had to rely on MRI to examine blood flow, Bashford said, but fTCD gives immediate feedback.
“MRI takes a while to get one static picture, or a series of pictures, and they represent time windows that are fixed,” Bashford said. “With fTCD, we are looking at the blood vessels in the brain and we’re watching in real time what happens; how they react to different stimuli. With the portability, non-invasiveness and silence, it makes it a nice technology to use when assessing how a patient is responding to the Galileo stimulation.”
There is still much to accomplish before this treatment can be made available to the masses, but Barlow and Bashford both said they believe this will be a game-changer for acute stroke care – one that is long overdue. Ischemic stroke accounts for 87 percent of all strokes, according to the American Stroke Association, and is the leading cause of long-term disability and fifth-leading cause of death in the United States.
“When you think about the number of stroke victims, and it spans all ages, it’s hard to overstate the impact this could have,” Bashford said.
Both researchers are also in varied stages of studying other applications for their technology, in addition to brain injuries. Barlow has already successfully applied somatosensory stimulation as an FDA-approved therapy for preterm infants to facilitate oral feeding skills, brain development, and better long-term learning outcomes. Bashford has applied fTCD to early detection of Alzheimer’s disease, and detection of emboli in infants with congenital heart disease undergoing surgery.
“I think we’re just scratching the surface with the rehabilitation possibilities,” Barlow said.