Jeff Wilkerson, April 29, 2019 | View original publication
In a bind: Team IDs potential cause of low testosterone
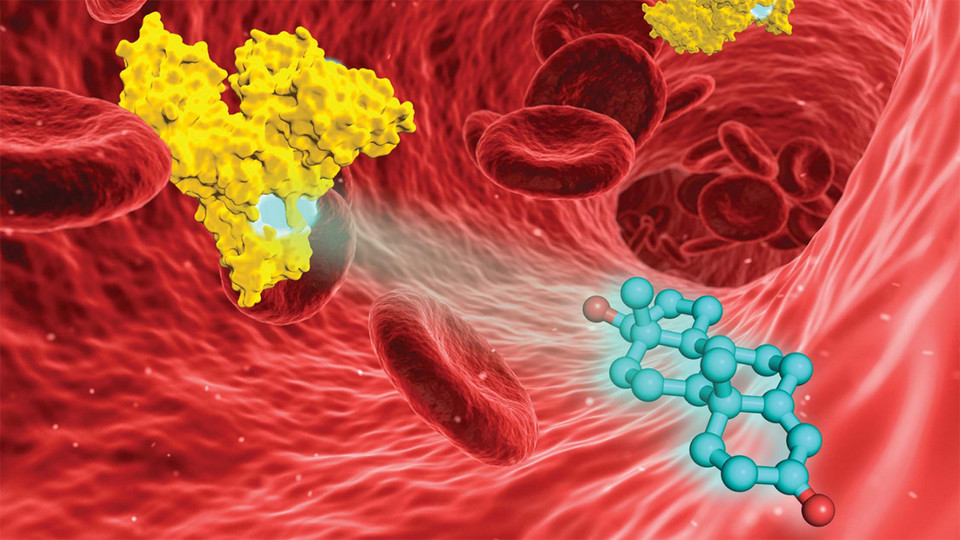
Competition for protein real estate in the bloodstream may explain why testosterone levels can drop among men who take certain medications or develop diabetes, says new research from the University of Virginia and University of Nebraska–Lincoln.
Prior studies have suggested that pain-relieving opioids such as methadone can markedly lower testosterone in men. And those contending with Type 2 diabetes are roughly twice as likely to see a decrease in active amounts of the male sex hormone.
While explanations have proven elusive, researchers do have an intriguing suspect: serum albumin, the blood’s most common protein and a known transporter of hormones, drugs and other agents hitching rides through the bloodstream.
Like most vehicles, serum albumin has designated seats for its passengers — certain regions that biological agents and pharmaceuticals can latch onto. Though roughly half of testosterone in the blood binds weakly with albumin — keeping the testosterone available for uptake by bodily tissues — researchers have struggled to identify which of the protein’s regions will accommodate the hormone.
Virginia’s Wladek Minor and his lab were equal to the task. By placing some testosterone-carrying serum albumin in a crystal, then bombarding the protein-hormone complex with X-rays and measuring how they diffracted, the team managed to identify two albumin regions to which testosterone will bind.
The catch? Those two regions of the protein also bind with many pharmaceutical drugs and can potentially interact with glucose molecules that are abundant in the bloodstreams of people with diabetes. In those scenarios, the testosterone normally gathered up by albumin effectively gets locked out and continues floating freely through the blood. It then becomes susceptible to getting picked up by a different blood protein that tightly straps in the hormone for the long haul, preventing it from taking the circulatory system’s exit ramps into the cells that can actually use it.
“So if you have someone who has low testosterone, and they’re also taking a high dosage of a drug that competes with the (serum albumin) sites the testosterone binds to, a change in testosterone levels might be tied into that competition,” said David Hage, Hewett University Professor of Chemistry at Nebraska. “You have to consider both at the same time.”
Ready for extraction
Hage has developed world-class techniques for analyzing how biological components interact with drugs and hormones under physiological conditions. So to get a better sense of how the proposed competition might play out in blood, Minor asked Hage to employ ultrafast affinity extraction, a technique the chemist pioneered at Nebraska a few years ago.
That technique involves a porous micro-scale column that can quickly bind to the drug or hormone of interest; a solution that simulates blood or a biological fluid; and small samples of whatever biological agents are being analyzed. As part of the study, Hage’s team allowed known quantities of testosterone and albumin to settle into a state of equilibrium, with some of the testosterone latching onto the albumin and some remaining free. The team also placed immobilized samples of albumin into the micro-column.
By rapidly passing the solution through the micro-column, then measuring how much testosterone got snagged by the albumin in that column, Hage’s team was able to calculate what proportion of the hormone had remained free at equilibrium. And by extending the amount of time that testosterone remained in the column, the researchers also measured how fast albumin releases testosterone from its grasp.
That information, coupled with the location of serum albumin’s binding sites, could eventually inform both the prescription of medications and the design of new ones, the researchers said. The ability to quickly analyze the behavior of an individual’s testosterone and albumin, meanwhile, points toward the potential for personalized treatments.
“If you know the relative extent of the binding, and you know the location of the binding,” Hage said, “you can start making some predictions about how the effective dosage of a testosterone treatment might change from one person to another.”
The researchers published their findings in the journal Chemical Science. Minor and Hage authored the study with Sandya Beeram, doctoral alumna of Nebraska; Kyungah Suh and Ashley Woolfork, graduate students in chemistry at Nebraska; along with the University of Virginia’s Ivan Shabalin, Mateusz Czub, Barat Venkataramany, Karolina Majorek Katarzyna Handing and Przemyslaw Porebski.
The team received support from the National Institutes of Health’s National Institute of General Medical Sciences under grants R01-GM044391, R01-GM117325, R01-GM117080 and R01-GM118619. The National Institute of Allergy and Infectious Diseases, National Institutes of Health, and the Department of Health and Human Services also funded the research under contracts HHSN272201200026C and HHSN272201700060C.