Tiffany Lee, November 5, 2020
Researchers aim to use protein to ramp up COVID-19 antigens’ impact
In the race to produce a COVID-19 vaccine, researchers around the world are using a wide range of strategies, from first-of-their-kind mRNA approaches to tried-and-true inactivated vaccines to oral, nasal and probiotic-based formulations.
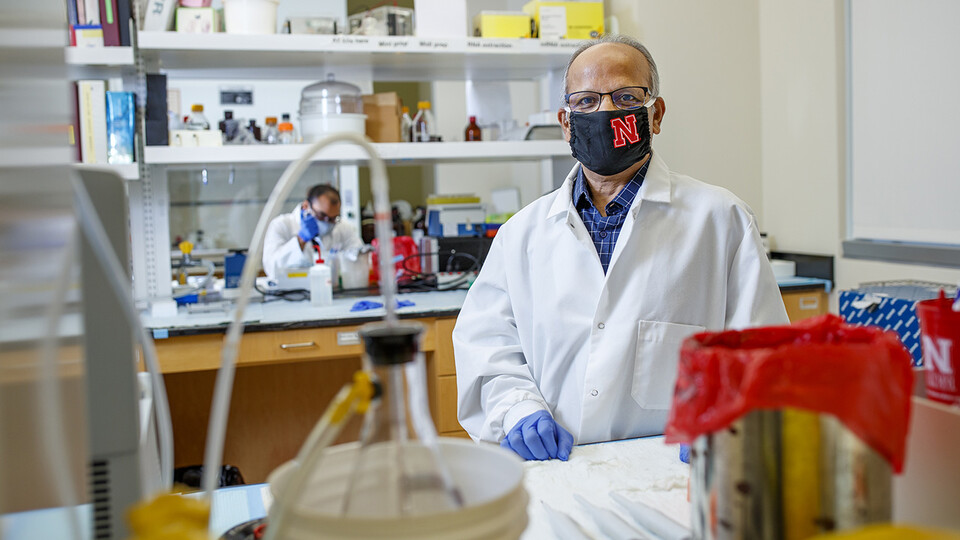
University of Nebraska–Lincoln virologist Asit Pattnaik is eyeing yet another approach. With support from the Office of Research and Economic Development’s COVID-19 Rapid Response Grant Program, Pattnaik is beginning to develop a vaccine framework that exploits the properties of a naturally occurring nanoparticle in an effort to produce a stronger, longer-lasting immune response than other vaccine candidates. He’s also taking a closer look at how SARS-CoV-2, the coronavirus that causes COVID-19, inhibits the immune system.
Tom Petro, professor of microbiology and immunology at the University of Nebraska Medical Center and a member of the Nebraska Center for Virology, is partnering with Pattnaik on the project.
The team’s vaccine work capitalizes on a protein called ferritin, which is produced by almost all living organisms. In humans, ferritin is the primary iron storage protein and guards against iron deficiency or surplus. It’s shaped like a symmetrical hollow sphere, or nanocage, built of 24 protein subunits. This cage structure, which Pattnaik calls a “spherical football,” makes ferritin unusually stable, allowing it to withstand variable temperatures and chemical environments.
To Pattnaik and Petro, ferritin’s well-organized, durable structure of 24 building blocks represents an opportunity to significantly ramp up the number of vaccine antigens — the molecules that trigger an immune response — delivered to a recipient. Their strategy is to fuse antigen to ferritin so that when the protein cage self-assembles, each nanoparticle will boast 24 molecules of the antigen on its surface, which is more than is found in many of the vaccines in development.
They are targeting SARS-CoV-2’s spike protein, known as the S protein, as the antigen. The S protein contains a region called the receptor-binding domain, which is key to the virus’s ability to enter the host cells and replicate.
“We are providing 24 molecules of receptor-binding domain in a single particle,” said Pattnaik, professor of veterinary medicine and biomedical sciences and a member of the Nebraska Center for Virology. “Such an approach will stimulate a more robust response than a single molecule would. And that’s the goal — to stimulate a better response.”
They believe that enhanced response will result from the higher antigen-to-immune cell ratio. The immune system’s antibody-producing B cells should trap the antigen-loaded nanoparticles, resulting in tighter and prolonged interactions that increase production and secretion of antibodies. The approach has been successful in producing strong antibody responses against viral pathogens such as influenza, HIV-1, Epstein-Barr virus and hepatitis C virus, among others.
A vaccine with stronger immunogenicity means people may need fewer doses. The current frontrunners would require at least two injections, spaced a month apart, to be effective. Pattnaik is hopeful that his approach would require fewer shots, which also means lower costs associated with supplies and administration.
The ORED grant is supporting Pattnaik and Petro as they try to clear the first major hurdle of their vaccine strategy — determining whether ferritin, fused with SARS-CoV-2’s S protein, triggers the strong production of neutralizing antibodies.
The team is also exploring the mechanisms by which SARS-CoV-2 causes aggressive and severe disease. Their hypothesis is that one of the virus’s most abundant proteins — the membrane protein, or M protein — suppresses the body’s innate immune response by thwarting activation of interferon regulatory factor 3. IRF3 plays a key role in spurring production of type 1 interferons, which, as their name suggests, are responsible for interfering with a virus’s life cycle.
Interferons have antiviral and anti-inflammatory properties and summon natural killer cells, a type of white blood cell that squashes infected cells, to the infection site. By stymying interferon production, the coronavirus may strip the body of its strongest natural defenses.
“What we’re trying to find out is whether we can understand more about the response of the host due to M protein expression, then target that response to develop therapeutics,” Pattnaik said.
The duo will study how M protein affects the antiviral response of human lung cells, with an eye toward developing a more comprehensive picture of how SARS-CoV-2 evades the immune system. Pattnaik hopes the research will lay the groundwork for developing effective anti-inflammatory treatments for COVID-19. Encouragingly, some interferon-based treatments have already been successful in treating COVID-19 patients.
Pattnaik said both components of his project are valuable in the global fight against COVID-19, which requires researchers to collaborate toward solutions.
“With this disease, we need experts from all different fields to put their efforts into developing effective therapeutics and vaccines.”