Tiffany Lee, November 10, 2020
Nasal spray could mean needle-free COVID-19 vaccine
As the world eagerly awaits the debut of a COVID-19 vaccine, many of us imagine that receiving the immunization will be similar to getting the flu shot: We’ll head to the clinic, roll up our sleeve and feel a quick prick to the arm.
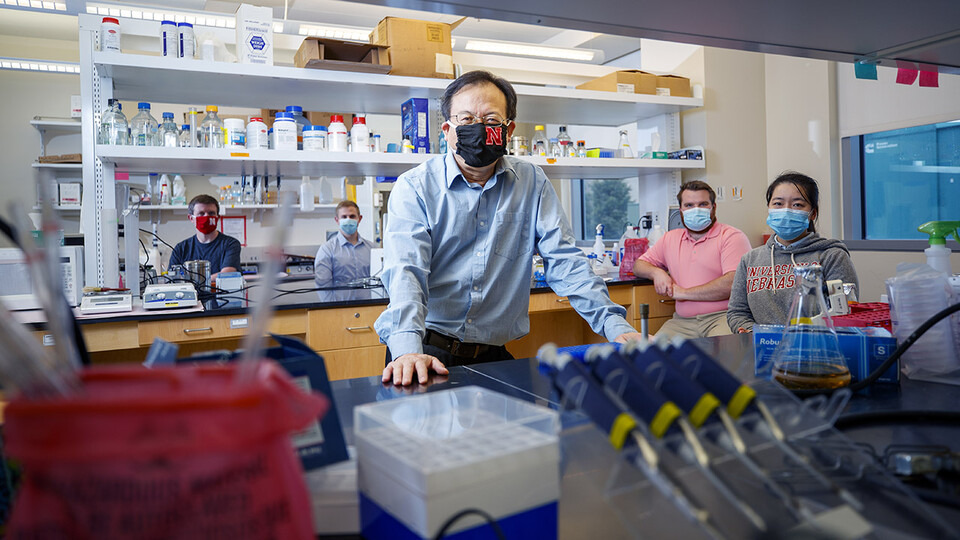
But Nebraska virologist Shi-Hua Xiang envisions a different approach, one with the potential to involve a little less pain and anxiety, enhanced immunity against COVID-19 and a smaller price tag.
With support from the Office of Research and Economic Development’s COVID-19 Rapid Response Grant Program, Xiang is in the early stages of developing a bacterial delivery system for a COVID-19 vaccine that would be delivered directly to the respiratory tract as a nasal spray, prompting an immune response directly at the site where SARS-CoV-2, the virus causing COVID-19, likely invades and multiplies.
Under Xiang’s approach, bioengineered Lactobacillus — a safe, widely used bacteria best recognized for its role in fermenting yogurt and cheese — would deliver antigens, the vaccine component that triggers an immune response, directly to the mucosal tissues of the nose and mouth. This site-specific strategy may provide more robust protection against COVID-19 than an injected vaccine because it would more closely mimic a natural COVID-19 infection, producing antibodies and immune cells in the key locations where the virus enters.
“Mucosal vaccination should be effective because mucosal vaccines induce immunity at the point of viral entry, controlling early infection before it becomes an established systemic infection,” said Xiang, associate professor of veterinary medicine and biomedical sciences and a member of the Nebraska Center for Virology.
With a spray vaccine, Xiang aims to capitalize on some of the uniquely powerful components of the body’s immune machinery that are located in mucosal tissues. The B cells there produce immunoglobulin A, or IgA, which is the body’s powerful first-line defense against pathogens in the gut and airway. Mucosal tissues are also rich in memory T cells, which are able to “remember” specific antigens after crossing paths with them the first time, enabling them to produce a faster, stronger immune response at the next encounter.
Xiang has studied Lactobacillus as a vaccine vector in the context of HIV, and he knows there are several advantages to its use. For one, as a food-based platform, it’s unquestionably safe: People routinely consume Lactobacillus in yogurt and other probiotic supplements. It’s also able to colonize the mucosal tracts, meaning it lives and multiplies in harmony with the airway’s other bacteria. Xiang hopes this means its protective effects will last longer, minimizing the number of times an individual needs the vaccination.
Lactobacillus is also relatively inexpensive to produce and amenable to genetic modification, meaning Xiang can genetically engineer the bacteria to produce SARS-CoV-2 antigens. This allows him to skip the costly and difficult process of antigen purification, which is required for traditional protein-based vaccines. There are other economic benefits to a nasal spray vaccine. It wouldn’t require needles, cutting equipment costs. And it wouldn’t necessarily require trained health care workers — people may be able to administer the nose spray themselves.
These characteristics make nasal spray vaccines a potentially viable solution for developing countries, which are struggling to secure doses of the leading COVID-19 vaccine candidates. Data show that developed nations have already agreed to purchase at least 3.7 billion doses of the most promising candidates, which experts say will monopolize global manufacturing capacity for the short term. And with only patchwork vaccine coverage globally, the pandemic will persist.
“One vaccine cannot cover the entire world,” Xiang said. “Different countries might need different vaccines. We need a variety.”
Accordingly, Xiang is also in the early phases of exploring a Lactobacillus-based COVID-19 vaccine: With the ORED grant, he’s using a pseudotyped COVID-19 virus to evaluate the effectiveness of the antibodies induced by the engineered bacteria. With about 45 vaccines already in clinical trials on humans, Xiang knows his work won’t contribute to a first-generation coronavirus vaccine. But with lingering questions about the frontrunners’ safety and success, and the developing world’s struggle to secure vaccines, he is confident his work will be valuable in the fight against COVID-19 and future viruses that jump from wildlife to humans.
“The long-term goal is to make an effective mucosal vaccine for respiratory-transmitted viral infections diseases,” Xiang said.