Veterinary Medicine and Biomedical Sciences
Scott Schrage, February 3, 2023
New vaccine platform could ease development, delivery of virus-fighters
To many, EV stands for “electric vehicle.” To researchers at Harvard University and the University of Nebraska–Lincoln, it’s shorthand for another vehicle — this one nanoscopic — that might help streamline the development and delivery of vaccines worldwide.
By repurposing one of the human body’s natural cargo transports, a Harvard-Nebraska team has developed a vaccine platform that could curb certain engineering challenges, storage demands and side effects of vaccines that combat HIV epidemics and the COVID-19 pandemic. The team’s platform also showed promise in early trials with mice, ramping up antibody production when pitted against HIV and improving survival rates in the face of influenza.
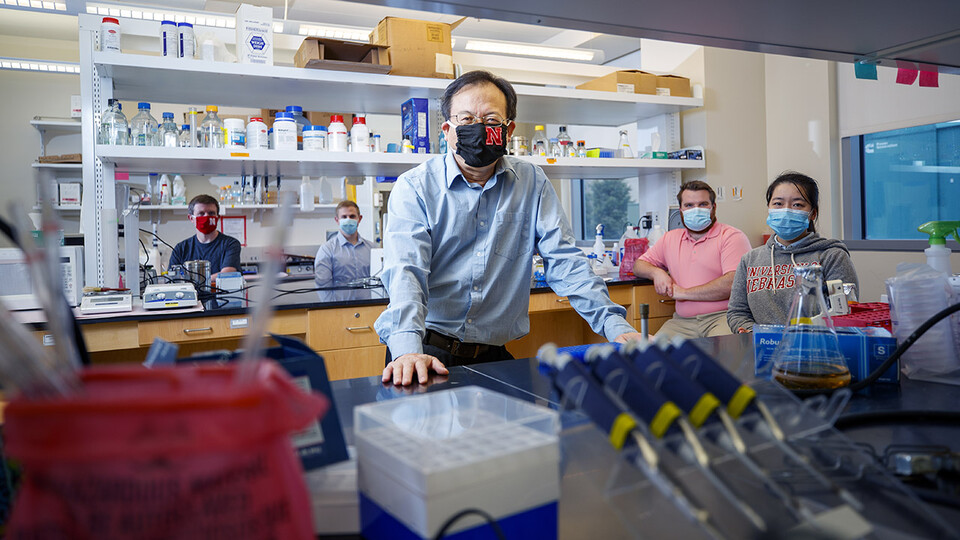
“We believe that this delivery system can enhance the immune response, particularly by inducing antibodies against viral infection,” said Shi-Hua Xiang, associate professor of veterinary medicine and biomedical sciences at Nebraska.
Historically, vaccines have consisted of weakened or inactivated viruses that are recognized by the human immune system, which responds with antibodies and cellular reinforcements that can remember and later fend off infectious forms of those viruses. For reasons of safety and effectiveness, though, many vaccines now instead consist of the lockpicking proteins that coat the surfaces of viruses — so-called antigens that the immune system recognizes as a threat to infiltrate cells.
But to stimulate recognition and immunity, the surface-level antigens in vaccines have to adopt the same three-dimensional poses they strike on viruses themselves. Unfortunately for vaccinologists, coaxing antigens into their native configurations can prove a difficult task. The genetic material of HIV, for instance, is enclosed in an envelope that also stabilizes one of the key proteins protruding from it. Persuading the protein to keep that configuration when uprooted from its viral foundation can mean pairing it with a similar surface or even splicing certain genes into its DNA, a feat that costs time and money.
Across 20-plus years of working on HIV vaccines, Xiang had often engaged in those feats of protein engineering himself. Then, in September 2017, Harvard’s Quan Lu visited Lincoln to give a seminar on a new type of extracellular vesicle: a nanoscopic particle, encased in a double layer of lipids, that ferries nucleic acids and other freight around the body. Xiang, who attended Lu’s talk, knew that lipid bilayers form the membranes of not just EVs and cells, but many viruses, too. The budding process that generated Lu’s EVs also resembled that of viruses. And EVs were roughly the same size as their viral counterparts. Those similarities got Xiang thinking.
“My thought,” he said, “was that maybe we could collaborate on a study.”
Alongside some colleagues, Xiang and Lu were soon looking into whether the latter’s new EV might recruit viral antigens to its surface, lock in their poses, and ultimately stimulate immune responses to them. The researchers started by introducing the EV to an influenza protein that, because of its presence across many different flu strains, has become the subject of the search for a universal flu vaccine. One particular domain of the EV not only drew in and fused with the flu antigen, it also helped promote the budding of more EVs than would otherwise be expected.
Encouraged, the team put its resulting EV to the test in mice. While mice facing the flu without a vaccine survived less than 30% of the time, those given three doses of the EV-based vaccine survived in 60-70% of cases. The vaccine was stimulating high levels of antibodies, the team found, with the antibodies then binding to and neutralizing the flu virus. When the researchers swapped out the flu antigen for an HIV protein, they again saw promising production of neutralizing antibodies in the serum of mice immunized with the vaccine.
Xiang said the platform may boast a couple of advantages even over mRNA vaccines — those that work by instructing cells to churn out antigens and have proven their worth against the SARS-CoV-2 virus responsible for COVID-19. Compared with the mRNA vaccines, which are shipped frozen and can be prone to breaking down over time, an EV-based vaccine will offer more stability and should remain viable at higher temperatures, he said.
Those advantages, Xiang said, could eventually push the EV platform to the forefront of vaccine design, production and delivery.
The team received support from the National Institutes of Health and reported its findings in the journal Science Advances. Lu and Xiang authored the study with Joshua Wiggins, a doctoral student at Nebraska, and Harvard University’s Sengjin Choi, Zhiping Yang, Qiyu Wang, Zhi Qiao and Maoyun Sun.